Monkeypox Vaccine, Side Effects Reason and Solution
After receiving the monkeypox vaccine, you developed a bump on your arm. Why this side effect is “very prevalent.”
Those who have received the monkeypox vaccine may be familiar with “the lump”. Since the virus epidemic reached the U.S. this summer. A lot of individuals have used social media to report the negative effects of the Jynneos vaccine. Which may be administered subcutaneously or intradermally (into the skin) (below the skin). A red bump at the injection site that lasts for two to three weeks is a typical complaint. It’s not a “strange” or “permanent” reaction, specialists say, nevertheless.
Any immunization may cause a brief lump to appear on your arm. But Anthony Fortenberry, a chief nursing officer notes that this reaction is most common with the Jynneos vaccine. This adverse effect is quite prevalent.
What brings on the bump?
The body’s immunological reaction to the monkeypox vaccine includes induration or a region of hardness at the injection site. According to Dr. Aditya Chandorkar, an assistant professor in the division of infectious diseases and international medicine at the University of Minnesota, “the body perceives the viral material as alien and sends immune cells to respond against it.” One of the effects of this response is a lump or swelling that results from some level of local reactivity. It’s crucial to understand that the existence or absence of swelling does not indicate how well the monkeypox vaccine will protect the individual.
Exist treatments for it?
Some patients have experienced bruising, soreness, itching, or tenderness on or near the lump due to the monkeypox vaccine. According to Fortenberry, “it usually does resolve on its own.” “Avoid scratching it at all costs because doing so can exacerbate the irritation, postpone healing, and even spread infection. And if it’s causing discomfort, over-the-counter Tylenol or Motrin are advised “in order to reduce inflammation.
How much time does it take to disappear?
It’s not unusual to experience a sizable, painless lump where the injection was given, according to Chandorkar. Over half of those who got the vaccination experienced. Some level of local swelling, according to the initial monkeypox vaccine study. Anecdotally, “In most cases, within a week to two weeks, the lump disappears. Most of the time, the lump should disappear on its own, negating the need for patients to visit a doctor.”

Despite having a lump, can I still take the second dose?
If the swelling has persisted for more than two weeks, there is no need to be concerned. Fortenberry claims that it is “very frequent” and shouldn’t dissuade individuals. By taking their second monkeypox vaccine dose four weeks following the first. According to Fortenberry, “so many patients have inflammation at the spot for several weeks.” Clinical advice (at vaccination sites) tackles the adverse effect of inflammation lasting up to four weeks. By instructing nurses to deliver the injection in the opposite arm

Monkeypox Virus view under Microscope
What are the other side effects of the Jynneos vaccine?
Muscle soreness, headaches, exhaustion, and nausea are among the more adverse effects of monkeypox according to Chandorkar. “Fever and chills are not common, despite reports to the contrary. Only 1% to 10% of patients exhibit them. According to him, the monkeypox vaccine‘s negative effects “are equivalent to most other vaccinations.” The majority of reactions are far milder than what some people reported after receiving the COVID-19 vaccinations.
When should you visit a doctor?
Dr Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine. He Advises patients to consult a doctor. If they experience fevers or chills for more than one to two days following the Jynneos vaccine. In regards to the lump, Hotez advises calling your doctor if the discomfort becomes bothersome. Or if you see the redness getting worse or spreading, even in streaks.
Although Fortenberry emphasizes that severe adverse reactions to the Jynneos vaccine are. Extremely rare, you should call 911 right away if you experience any of the following symptoms. After receiving the vaccine. Difficulty breathing, hives, swelling of the face or throat, a fast heartbeat, dizziness, or weakness.
Why is immunization a necessity?
Even while unpleasant side effects like the lump might seem preferable to the alternative of contracting. Monkeypox, which is a painful infection with symptoms that can persist for two to four weeks. And necessitates quarantine, side effects are far preferable. The best method to prevent infection, according to Hotez, is to be vaccinated. Although seldom deadly, monkeypox is a dangerous and incapacitating infectious illness that may necessitate hospitalization.
Additionally, do not be afraid to speak with the medical staff at the immunisation location. If you are concerned about any potential adverse effects. They have all the information needed to reassure people. They guarantee that everyone has very clear expectations regarding the vaccine, according to Fortenberry. “If a second dosage is available, we urge everyone to finish their vaccination series. Don’t allow adverse effects to stop you from receiving the second dose and gaining complete immunity from monkeypox. If you have any questions or concerns, it’s crucial to contact a medical professional; that’s what we’re here for. “With the internet, you don’t have to handle things on your own.”
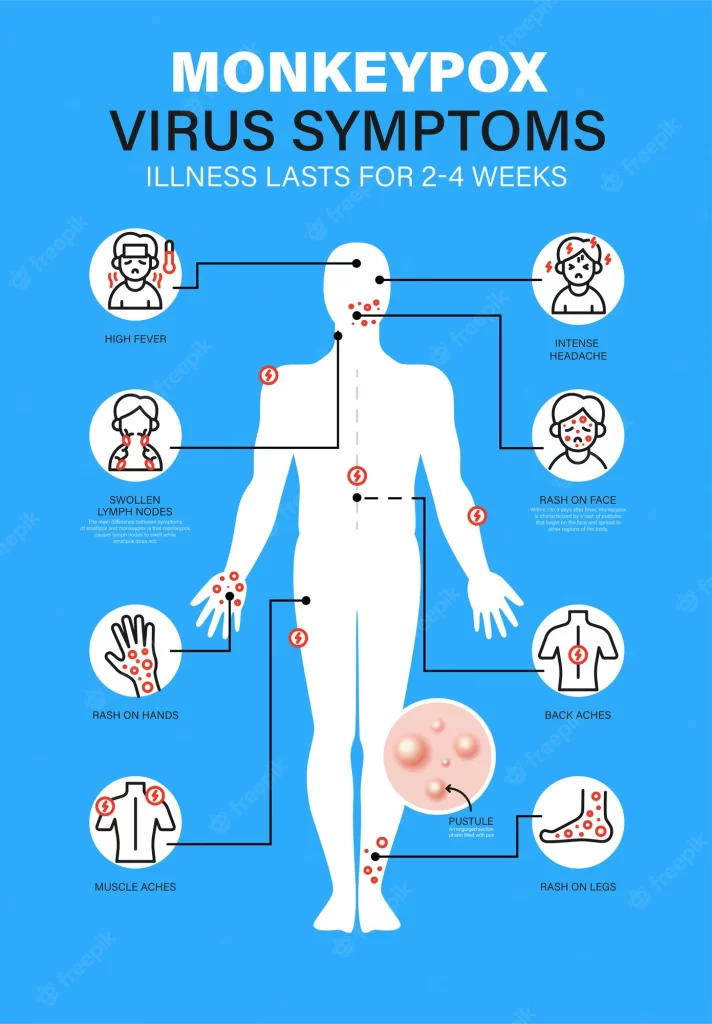
What are the symptoms? you need to know before monkeypox affects you.
According to the Centres for Disease Control and Prevention. The uncommon condition known as monkeypox is brought on by the monkeypox virus. A member of the same orthopoxvirus genus and poxvirus family as the more dangerous and contagious smallpox virus. Although it will cause lymph nodes to enlarge and is often less serious than smallpox. The monkeypox is recognised for a distinctive rash and presents similarly to smallpox.
Monkeypox is a zoonosis, meaning that the virus is transmitted to people from animals. People typically become infected sporadically in the forested parts of Central and West Africa. After an interaction with an infected animal. Once infected, people can spread the virus to others, but that requires close contact. The monkeypox name stems from the disease’s discovery in lab monkeys in 1958. But the monkeypox virus is not found exclusively or even primarily in monkeys. Many species, including rope and tree squirrels, Gambian pouched rats, and dormice, are able to harbour the monkeypox virus. The natural host and source of the virus is unknown but is likely to be a rodent.
There are two main types of monkeypox virus. A West African version or “clade,” which is less severe and is the virus identified in the latest outbreak. And another is more lethal Congo Basin clade.
The number of people diagnosed with Monkeypox (MPX) in Victoria is increasing due to local transmission.
— VicGovDH (@VicGovDH) August 26, 2022
Preventive measures including limiting sexual partners are very important for people who are not vaccinated.
For more information, visit: https://t.co/pbeCmj3vur pic.twitter.com/LbcCv4kvb0
1. It’s caused by a smallpox-like virus
The same virus that causes smallpox, which is now completely wiped from the earth, also causes monkeypox. Both belong to the family Poxviridae’s Orthopoxvirus genus. When outbreaks of a disease producing a pox were found in captive monkeys used for study, monkeypox was first identified. In the Democratic Republic of the Congo (DRC), where it was originally discovered across 1970. It is now endemic in Central and West Africa. 2020 saw 4,594 probable cases of monkeypox recorded by the World Health Organisation (WHO). With 171 fatalities (case fatality ratio 3.7%). They are referred to as suspected since PCR testing, which is required for confirmation. So it is difficult to get in endemic locations.
2. It causes pustules all over the body
Although it might take up to 21 days, symptoms often start to manifest five to 13 days after infection. Fever, headache, muscular aches, backaches, enlarged lymph nodes, chills, and tiredness are some of the early symptoms. When a fever first appears, a rash usually breaks out first. By concentrating on the hands, feet, and face before moving to other parts of the body. It has the potential to spread to the eye, genitalia, and the interior of the mouth. The rash worsens until a scab forms and falls off. In certain circumstances, big chunks of skin might also come off the body. Symptoms frequently subside after a month, but one out of every ten instances might be deadly. Children are especially vulnerable.
3. Diagnosis requires PCR tests
Given that many other illnesses, including chickenpox and measles, can cause rashes, the WHO advises diagnosis when identification is required. They assert that this can only be done using PCR testing. Since orthopoxviruses can create antigens and antibodies that resemble those of other related viruses. Therefore tests of these cannot identify the virus as monkeypox.
4. It can spread between people through close contact
Infected wild animals like rats and monkeys. Found in the rainforests of Central and West Africa often transmit the virus to humans. Although human-to-human transmission is also possible. Similar to viruses like Ebola. Transmission only occurs when infected objects, such as contaminated bedding or clothing. Come into contact with lesions, bodily fluids, respiratory droplets, or both.
5. There’s currently no cure, but we have a (very old) vaccine
WHO does not currently propose a particular therapy for monkeypox. However antivirals like tecovirimat that are approved to fight orthopoxviruses do exist. Years ago, the smallpox vaccine was essential to the eradication of smallpox, and it is 85% effective in preventing monkeypox. The first-generation smallpox vaccinations, however, are no longer offered to the general population. For the protection of smallpox and monkeypox. A more recent monkeypox vaccine based on vaccinia was licensed in 2019, however it is also not yet widely accessible.
You can read more about Human Monkeypox virus in link given below.
- Related Tags: a picture of monkeypoxabout monkeypox virusafrica monkeypoxare monkeypox contagiousare monkeypox deadlyare monkeypox from monkeysare monkeypox itchyatlanta monkeypoxaustralia monkeypoxaustralia monkeypox casesbavarian nordic monkeypoxbbc news monkeypoxbc monkeypoxbelgium lockdown monkeypoxbelgium monkeypoxberlin monkeypoxbno monkeypoxboston monkeypoxbreaking news monkeypoxbroward monkeypoxcan monkeypox be curedcan monkeypox kill youcan u die from monkeypoxcanada monkeypoxcauses of monkeypoxcdc monkeypoxcdc monkeypox 2022cdc monkeypox outbreakchickenpox vs monkeypoxcure for monkeypoxdallas monkeypoxdifference between chickenpox and monkeypoxdo monkeypox itchdoes monkeypox come from monkeysdoes monkeypox go awaydoes monkeypox itchdoes monkeypox killdoes monkeypox kill youdoes monkeypox leave scarsdoes monkeypox vaccine prevent monkeypox?does smallpox vaccine prevent monkeypoxearly monkeypox rashecdc monkeypox early signs of monkeypoxeffective monkeypox vaccineeurope monkeypoxmonkeypoxmonkeypox airbornemonkeypox alabamamonkeypox anaheimmonkeypox and eczemamonkeypox and pregnancymonkeypox arizonamonkeypox arkansasmonkeypox atlantamonkeypox atlanta casesmonkeypox austinmonkeypox bay areamonkeypox berkeleymonkeypox blindnessmonkeypox blistersmonkeypox boisemonkeypox bostonmonkeypox bouldermonkeypox brooklynmonkeypox bumpsmonkeypox by statemonkeypox californiamonkeypox casesmonkeypox cases in californiamonkeypox cases in floridamonkeypox cases in texasmonkeypox cases in usmonkeypox cases worldwidemonkeypox cdcmonkeypox chicagomonkeypox curemonkeypox dallasmonkeypox day 1monkeypox dcmonkeypox deadlymonkeypox death tollmonkeypox deathsmonkeypox definitionmonkeypox delawaremonkeypox denvermonkeypox detroitmonkeypox early rashmonkeypox early stagesmonkeypox early symptomsmonkeypox eczemamonkeypox effectsmonkeypox el pasomonkeypox emergencymonkeypox endemicmonkeypox epidemicmonkeypox europemonkeypox explainedmonkeypox new yorkmonkeypox newsmonkeypox nycmonkeypox outbreakmonkeypox outbreak 2022monkeypox pandemicmonkeypox rashmonkeypox symptomsmonkeypox transmissionmonkeypox treatmentmonkeypox ukmonkeypox usmonkeypox vaccinemonkeypox vaccine administrationmonkeypox vaccine mandatemonkeypox vaccine near memonkeypox vaccine nycmonkeypox vaccine usamonkeypox virusmonkeypox virus newsmonkeypox virus vaccinesmallpox vaccineuk monkeypoxvaccinevaccineswhat is monkeypox
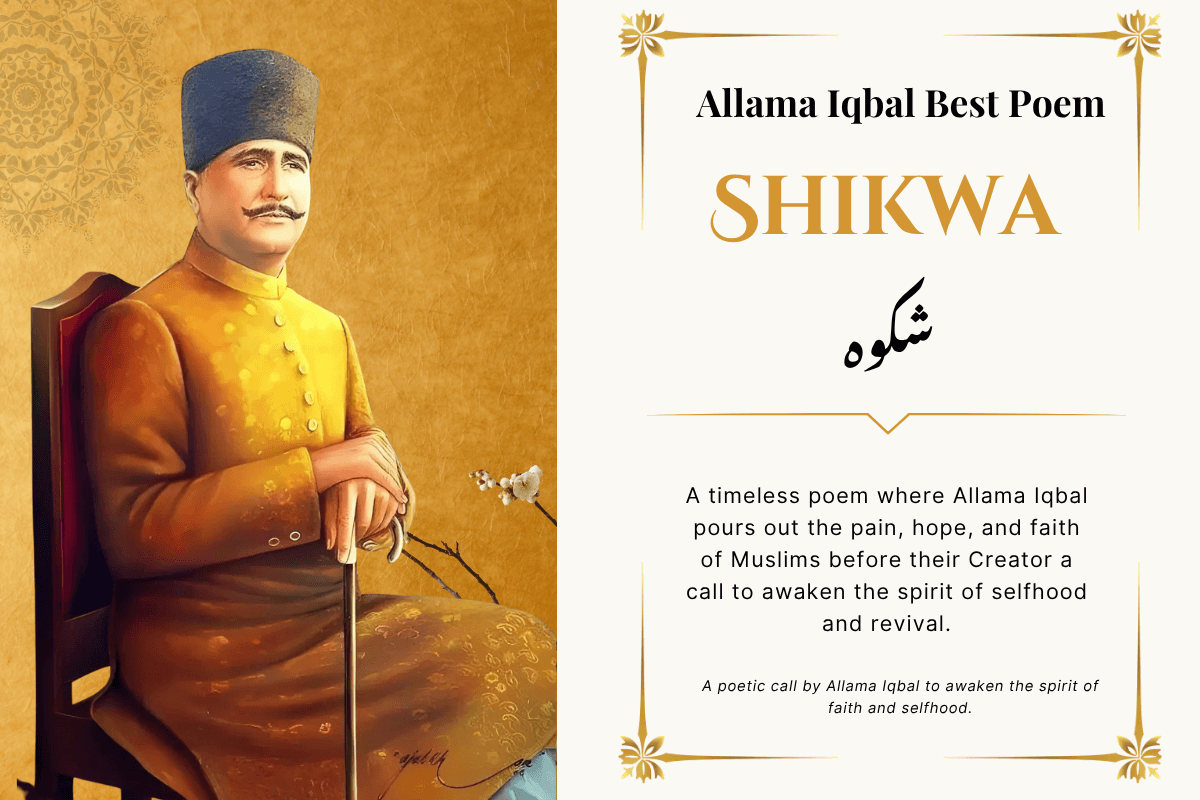
Allama Iqbal Shikwa Poem
Poetry Allama Iqbal Urdu
Hawaii Artificial Intelligence
Solar Energy Price in Pakistan
iPhone 17 pro max
Enjoy this post? Join our newsletter
Don’t forget to share it
Related Articles